Highlights of the 2022 Medicare Physician Fee Schedule
Recently, the Centers for Medicare & Medicaid Services released the 2022 Medicare Physician Fee Schedule final rule. To assist our members in deciphering the rule we have created a highlights document outlining several provisions finalized for 2022. If you have questions about the rule or other clinical practice payment and policy questions, please contact IDSA staff at clinicalaffairs@idsociety.org.
CMS to Apply MIPS Automatic Extreme and Uncontrollable Circumstances Policy for the 2021 Performance Year in Response to COVID-19 Public Health Emergency
CMS will apply the Automatic Extreme and Uncontrollable Circumstances Exemption Policy (EUC) for the 2021 MIPS performance year. This 2021 policy change recognizes the continued challenges physicians face with providing care during the PHE and reduces administrative burden. Therefore, if a physician participates in MIPS as an individual, they don’t need to take any action to have the automatic EUC policy applied to them. CMS will automatically identify and re-weight all 4 MIPS performance categories reweighted to 0% and receive a neutral payment adjustment for the 2023 MIPS payment year unless the physician:
- Submit data in 2 or more performance categories, or
- Have a higher final score from group or APM Entity participation
Unfortunately, due to a systems issue if a physician or small practice participates in the 2021 MIPS program by submitting Part B quality measures through claims and has submitted quality data codes on their 2021 Medicare claims, they will need to still file a 2021 MIPS Hardship EUC to avoid a 2023 payment adjustment and be exempt from the 2021 MIPS program.
If a group practice that typically participates in MIPS as a group has not submitted 2021 data, then the automatic EUC policy will apply to the individual physicians within the group. If the group has submitted any 2021 data, then they will need to apply for the EUC to avoid a 2023 payment adjustment.
Essentially, if the physician or practice has not submitted any 2021 MIPS performance data, then the automatic EUC will apply to the physician.
PY2021 EUC Exception Applications can be submitted by signing in to qpp.cms.gov and clicking Exception Applications on the left-hand navigation.
For more detailed information, please the CMS announcement.
CMS Releases the 2022 Medicare Physician Fee Schedule and Quality Payment Program Final Rules
On November 2, 2021, the Centers for Medicare & Medicaid Services (CMS) released the 2022 Medicare Physician Fee Schedule final rule and the associated Fact Sheet . The rule also includes finalized polices for the 2022 Quality Payment Program.
IDSA staff along with members of the Clinical Affairs Committee and the Payment Policy Work Group will review the rule for policies and proposals that effect IDSA members. Of note, the Agency mentions the IDSA outbreak activation concept and the associated creation of a modifier to pay for items, services and other work associated with a pandemic that go above and beyond patient care. We have been working on this policy initiative since the beginning of the pandemic and believe that this is a step in the right direction. We will continue to work with CMS staff to develop this concept.
IDSA will be looking closely at final policies associated with evaluation and management services, telehealth services, direct billing for services provide by physician assistants. If you have any questions about the rule, please contact the Clinical Affairs Department at clinicalaffairs@idsociety.org.
MIPS Facility-Based Scoring Is Not Available for Performance Year (PY) 2021
In response to the impact of the ongoing COVID-19 public health emergency (PHE), CMS finalized a measure suppression policy in the Fiscal Year (FY) 2022 Inpatient Prospective Payment System (IPPS)/Long-Term Care Hospital (LTCH) PPS final rule for several hospital reporting programs, including the Hospital Value-Based Purchasing (VBP) Program. This policy allows CMS to suppress the use of measure data if the agency determines that circumstances caused by the COVID-19 PHE have affected those measures and the resulting quality scores significantly. CMS has also finalized the suppression of 7 measures for the FY 2022 Hospital VBP Program under this policy.
CMS believes that calculating a total performance score in the Hospital VBP Program for hospitals using only data from the remaining measures, all of which are in the Clinical Outcomes Domain, wouldn’t result in a fair national comparison. Therefore, CMS finalized a special scoring policy for FY 2022 that won’t calculate a total performance score for any hospital for FY 2022.
How does this affect MIPS facility-based scoring in PY 2021?
The total performance score from the Hospital VBP Program to calculate Merit-based Incentive Payment System (MIPS) facility-based scores for facility-based clinicians and groups in the quality and cost performance categories. The FY 2022 total performance score is what CMS would use to determine these scores for the 2021 MIPS performance year.
- Because the FY 2022 total performance score from the Hospital VBP Program won’t be available, CMS won’t be able to calculate MIPS facility-based scores for the 2021 MIPS performance year.
What does this mean for MIPS reporting?
Facility-based clinicians and groups will need to submit data on MIPS quality measures (except for administrative claims-based measures that have a benchmark, which are automatically calculated for clinicians and groups that meet the case minimum) to receive a score other than zero for the quality performance category.
CMS will automatically calculate a score for the cost performance category for facility-based clinicians and groups that meet the case minimum for at least one MIPS cost measure; there are no data collection or submission requirements for the cost performance category. If the facility-based clinician or group doesn’t meet the case minimum for any cost measures, the cost performance category will be reweighted to 0% and the weight redistributed to other performance categories.
- Facility-based clinicians and groups without available and applicable measures can request performance category reweighting by submitting an extreme and uncontrollable circumstances (EUC) application.
- Please be sure to cite “COVID-19” as the triggering event,as the decision to suppress measures in the Hospital VBP Program was in response to the COVID-19 PHE.
Additional Resources
- For more information on the policies in the IPPS final rule, please refer to 86 FR 45295 in the published version of the rule on the Federal Register.
- For more information on available quality measures, please visit the Explore Measures and Activities tool.
- The following resources are available on the QPP Resource Library:
- For more information on reporting MIPS quality measures, please review the 2021 Quality Quick Start Guide (PDF) or 2021 MIPS Quality User Guide (PDF).
- For more information on the MIPS cost performance category, please review the 2021 MIPS Cost User Guide (PDF).
- For more information on the EUC application, please review the 2021 MIPS Extreme and Uncontrollable Circumstance Exception Application Guide (PDF).
- We’ve also updated the 2021 Facility-Based Quick Start Guide (PDF) to reflect this information.
Quality Payment Program (as Required by MACRA)
The Centers for Medicare & Medicaid Services (CMS) began the Quality Payment Program (QPP) on January 1, 2017. The QPP fulfills the mandate of the Medicare Access and CHIP Reauthorization Act (MACRA) to implement an incentive program that rewards Medicare-participating clinicians for high quality, cost efficient, value-based care. The QPP comprises two tracks: the Merit-Based Incentive Payment System (MIPS) and the Advanced Alternative Payment Models (APMs). ID physicians may choose which track to participate in based on practice size, location, or patient population.
Most ID physicians will participate in the MIPS. For information on your MIPS eligibility, enter your 10-digit National Provider Identifier (NPI) into the CMS QPP Participation Status tool.
CMS updates the Quality Payment Program and physician payment formulas annually, typically through issuing first a proposed rule, on which it receives public comment, and then a final rule. IDSA continually submits comment letters to CMS on the proposed and final QPP/ Physician fee schedule rules advcoating on behalf of our members.
The Merit-Based Incentive Payment System (MIPS) is a performance-based payment program for clinicians who bill under Medicare Part B and meet the minimum volume threshold requirements implemented by CMS. Clinicians participating in MIPS are evaluated based on four separate categories:
- Quality: Clinicians must select and report on quality measures that evaluate care processes and patient outcomes.
- Improvement Activities: Activities or programs that may improve clinical practice or care delivery, and that will likely result in improved patient outcomes. Clinicians must select at least two from a list updated annually by CMS.
- Promoting Interoperability: Measures of effective electronic health record technology. The use of Certified Electronic health record technology (CEHRT) is required.
- Cost: CMS scores clinicians on multiple cost measures, based on data already submitted through the Medicare administrative claims process for an entire performance year.
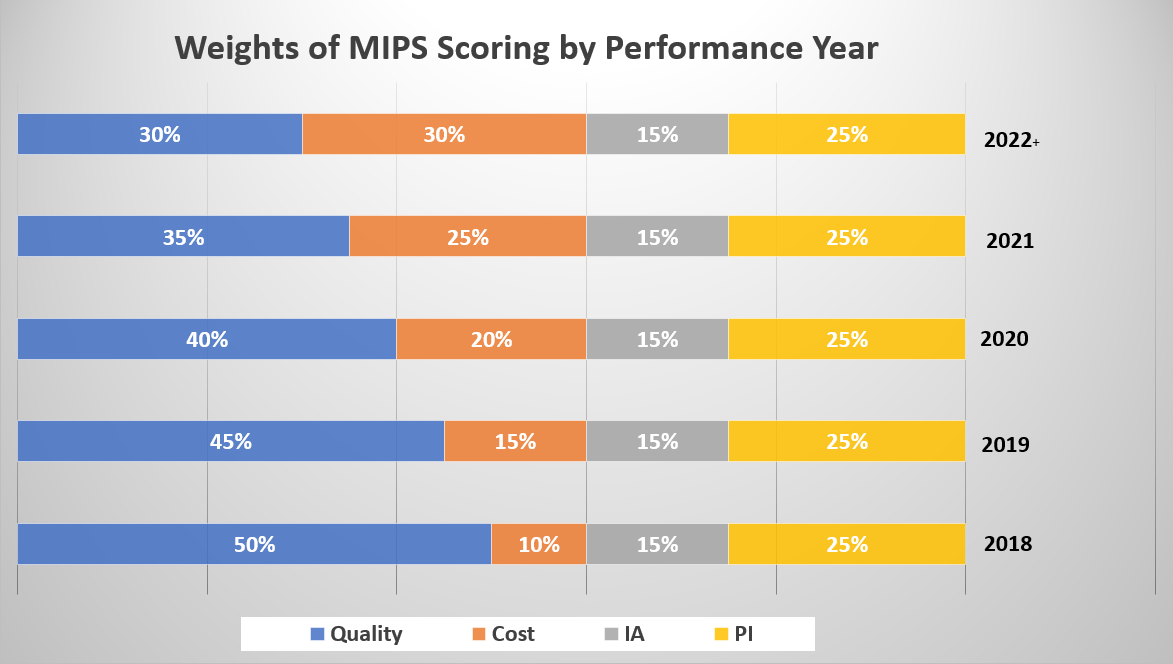
Data for MIPS can be reported at the individual clinician or group practice level. CMS combines performance in each of the four categories to create a composite score to assess overall performance and determine the applicable payment adjustment. There is a two-year lag between the year for which the data are collected—the performance year—and the payment impact (i.e., quality scores collected in performance year 2018 will affect payment in 2020). See the chart below to determine the relative weighting of each category by performance year.
CMS will report on the public Physician Compare website the clinician or group's scores for each category, as well as the final score.
IDSA is aware of the lack of applicable quality measures to the ID physician and has voiced concerns to CMS regarding this troubling issue. IDSA is currently exploring initiatives to address the inappropriate evaluation of ID physicians. IDSA suggests to report on the following measures, depending on where the physician sees patients:
- Measure #110: Preventive Care and Screening Influenza Immunization
- Measure #111: Pneumococcal Vaccination Status for Older Adults
- Measure #128: Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow-Up Plan
- *Measure #130: Documentation of Current Medications in the Medical Record
- Measure #226: Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
- Measure #474: Zoster (Shingles) Vaccination
- Measure #475: HIV Screening
*Indicates high-priority measures
For more details, please use the CMS QPP explore quality-measures tool.
Clinical Practice Improvement Activities
As a part of the MIPS, CMS will also measure the use and reporting of clinical practice improvement activities, which is a new quality measurement category. Improvement activities are activities (such as expanded practice access) or programs (such as antibiotic stewardship) that may improve clinical practice or care delivery and that will likely result in improved outcomes.
Under the new MIPS program, providers can chose from a list of 90+ improvement activities (IAs) in order to meet the requirements of the improvement activity category. IDSA has prepared a list of improvement activities that ID physicians may wish to report. For the first year of the program, in order to avoid a penalty, a provider only needs to report and attest to one improvement activity. IDSA encourages physicians to review the entire list of improvement activities from the Quality Payment Program website.
Providers will need to attest that an improvement activity was performed. CMS has stated that while they’re not requiring physicians to submit any documentation to prove an IA was completed, physicians are encouraged to retain medical records or any other data used to support/determine the completion of the activity for up to 10 years following the performance period.
Example of MIPS Clinical Practice Improvement Activities
- Patient Safety and Practice Assessment: Implementation of an antibiotic stewardship program that measures the appropriate use of antibiotics for several different conditions (URI Rx in children, diagnosis of pharyngitis, Bronchitis Rx in adults) according to clinical guidelines for diagnostics and therapeutics
- Expanded Practice Access: Use of telehealth services and analysis of data for quality improvement, such as participation in remote specialty care consults, or teleaudiology pilots that assess ability to still deliver quality care to patients.
- Emergency Response and Preparedness: Participation in Disaster Medical Assistance Teams, or Community Emergency Responder Teams. MIPS eligible clinicians and MIPS eligible clinician groups must be registered for a minimum of 6 months as a volunteer for disaster or emergency response.
- Population Management: Manage medications to maximize efficiency, effectiveness and safety that could include one or more of the following: Reconcile and coordinate medications and provide medication management across transitions of care settings and eligible clinicians or groups; Integrate a pharmacist into the care team; and/or conduct periodic, structured medication reviews.
- Population Management: Participation in research that identifies interventions, tools or processes that can improve a targeted patient population.
- Population Management: Participation in a QCDR, clinical data registries, or other registries run by other government agencies such as FDA, or private entities such as a hospital or medical or surgical society. Activity must include use of QCDR data for quality improvement (e.g., comparative analysis across specific patient populations for adverse outcomes after an outpatient surgical procedure and corrective steps to address adverse outcome).
Additional Resources
The CMS QPP Experience Report provides a comprehensive representation of the overall clinician experience during QPP performance years with the latest available data to help healthcare professionals understand trends in QPP performance and reporting. Additionally, the QPP Experience Report Public Use Files (PUF) provide further details on QPP participation data.
If you have questions or need assistance with MIPS reporting please contact the Quality Payment Program Service Center.
The help desk is available Monday – Friday; 8:00 AM–8:00 PM ET:
Phone: 1-866-288-8292 TTY: 1-877-715-6222 Email: QPP@cms.hhs.gov
Facility-based measurement offers MIPS eligible clinicians and groups the opportunity to receive scores in the MIPS quality and cost performance categories based on the FY 2022 score for the Hospital Value-Based Purchasing (VBP) Program earned by their assigned facility.
Individual MIPS eligible clinicians qualify for facility-based measurement in the 2021 MIPS performance period when they:
- Billed at least 75% of their covered professional services in a hospital setting (inpatient hospital (Place of Service (POS)=21), oncampus outpatient hospital (POS=22), or emergency room (POS=23)) between October 1, 2019 and September 30, 2020;
- Billed at least one service in an inpatient hospital or emergency room between October 1, 2019 and September 30, 2020; and
- Can be assigned to a facility with a FY 2022 Hospital VBP Program score. (Note that we won’t know if a facility has a FY 2022 score until Fall 2021 at the earliest.)
Groups qualify for facility-based measurement in the 2021 MIPS performance period when:
- More than 75% of the clinicians in the practice qualify for facility-based measurement as individuals
For more information on MIPS facility-based measurement and how to check if you qualify, please review the 2021 Facility-Based Quick Start Guide.
Alternative Payment Models (APMs)
Alternative Payment Models are arrangements that reward participants for providing high-quality cost-effective care. Alternative Payment Models can apply to a specific condition, care episode, or population, and typically rely on care coordination and integration to achieve better results for their patients. CMS designates two kinds of Alternative Payment Models within the Quality Payment Program:
- MIPS APMs: These models include MIPS-eligible clinicians and provide financial incentives for performance on cost, utilization, and/or quality measures at either the participating clinician or APM entity level. Physicians who participate in an MIPS APM are still evaluated on the four MIPS domains (quality, improvement activities, cost, and promoting interoperability), but the MIPS APM performance category weighting differs from the general MIPS scoring methodology, assigning “cost” a category weight of zero and providing higher weights for quality, improvement activities, and promoting interoperability. Unlike the general MIPS program, these weights do not change from year to year. MIPS APMs also allow participants to use quality measure reporting at the APM level, reducing the quality measure reporting burden for the individual physician or practice.
- Advanced APMs: These APMs also hold participants responsible for performance on cost and quality, but in addition require participants to assume downside financial risk. Advanced APM participants must also use 2015 Certified Electronic Health Record Technology (CEHRT). In exchange, Advanced Alternative Payment Models offer a 5% bonus, and allow clinicians to be excluded from MIPS reporting requirements. The APM itself will also offer APM-specific rewards based on its design. Clinicians can be eligible for advanced APMs if they meet certain threshold requirements for percentage of Medicare patients/percentage of Medicare Part B payments receiving care through the Advanced APM.
For more information, refer to the list of care models designated as MIPS APMs and Advanced APMs.
QPP Resources
The American Medical Association (AMA) offers podcasts, learning modules, and webinars to help physicians and their staff prepare for participation in the QPP.
Home Infusion Therapy Services
Medicare Learning Network article that provides guidance to providers and suppliers of home infusion therapy services about claims processing systems.
Medicare Utilization Data for Infectious Diseases Physicians
Please visit the Medicare Research, Statistics, Data & Systems Page for free and purchasable information, including utilization rates, cost reports, error rates, and beneficiary and provider surveys.

